The Complete Medical Billing Workflow
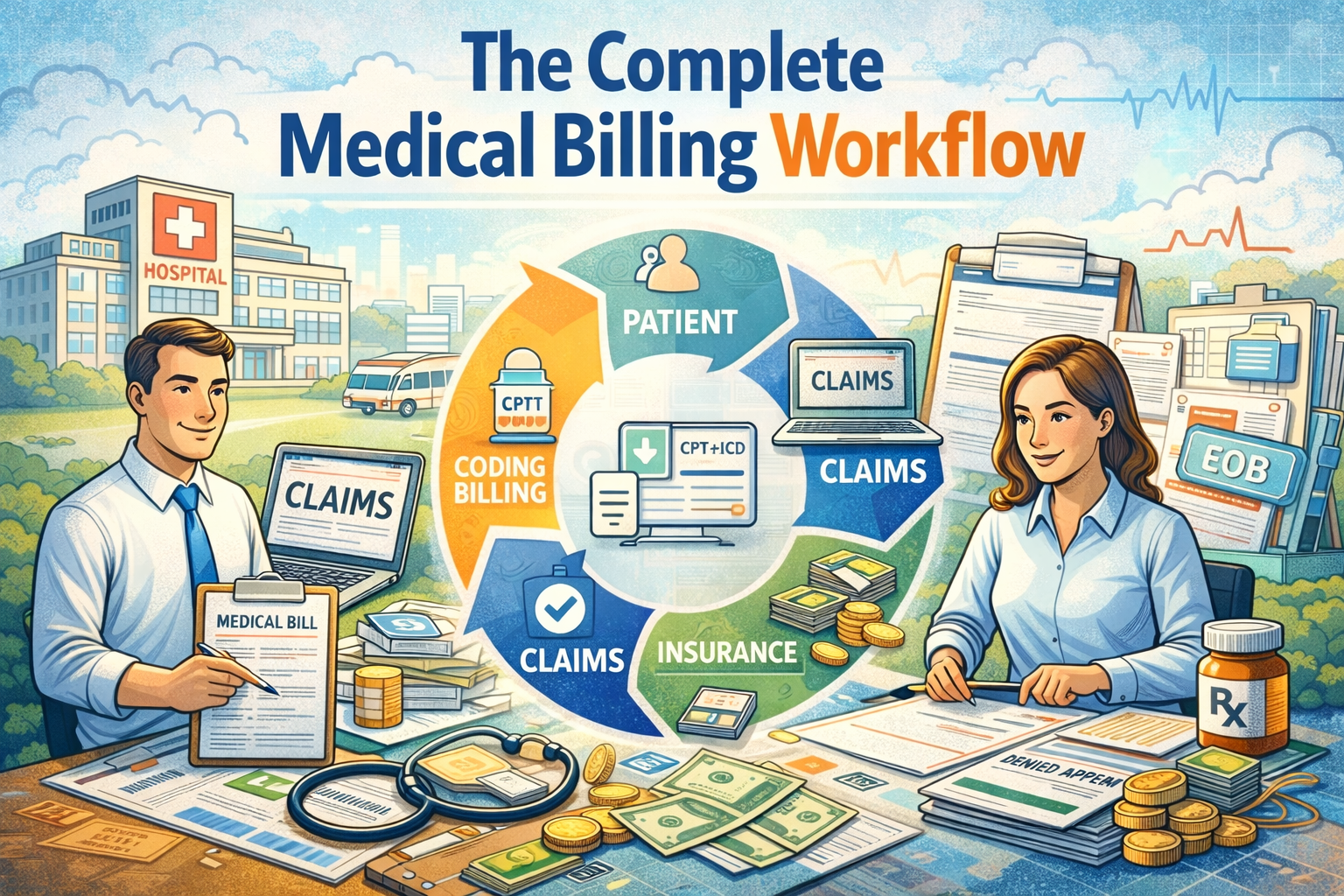
Learn how patient registration, insurance verification, medical coding, claim submission, payment posting, and denial management work together to create a clean revenue cycle.
What Is Medical Billing?
Medical billing is the process of translating healthcare services into claims that insurance companies can understand and reimburse. It is a key component of Revenue Cycle Management (RCM) and involves multiple stages that must be executed accurately to ensure timely payment. Understanding the medical billing workflow is essential for billers, coders, healthcare administrators, and anyone working in medical office operations.
Popular Keywords included naturally:
✔ medical billing process
✔ revenue cycle management (RCM)
✔ clean claim
✔ healthcare reimbursement
✔ medical billing workflow
1. Patient Registration: The First Step in the Medical Billing Process
Patient registration is the foundation of the revenue cycle. During this stage, the front desk team collects essential patient demographics, including name, contact details, date of birth, address, and emergency contact information. These details must be accurate because they directly affect the claim approval process.
The staff also obtains and scans insurance cards, identifies primary and secondary insurance, and verifies policyholder information. Patients sign important documents such as HIPAA consent, financial responsibility agreements, and assignment of benefits. These forms protect the provider legally and financially.
A single spelling mistake or outdated insurance detail can result in a claim rejection, making this step crucial for creating a clean claim submission later.
Keywords Added:
✔ patient demographics
✔ assignment of benefits (AOB)
✔ clean claims
✔ HIPAA consent
✔ front-end medical billing
2. Insurance Verification: Ensuring Active Coverage Before Service
Insurance verification is one of the most important steps in medical billing because it prevents unnecessary denials. During this stage, medical billing staff confirm whether the patient’s insurance policy is active on the date of service.
They check:
– coverage eligibility
– copay, deductible, and coinsurance
– referral or prior authorization requirements
– plan limitations
– in-network or out-of-network status
Insurance verification teams often use payer portals, eligibility checking tools, and clearinghouse platforms to verify benefits. By completing this step accurately, providers prevent eligibility denials, authorization denials, and unpaid claims, which are some of the most common reasons for lost revenue in healthcare.
Keywords Added:
✔ insurance eligibility verification
✔ prior authorization
✔ eligibility denials
✔ payer portals
✔ insurance benefits verification
3. Charge Entry: Converting Services Into Billable Charges
Once the patient encounter is complete, the medical billing team begins charge entry, which involves entering the provider’s documented services into the billing system. This process uses information from encounter forms, superbills, or EHR documentation.
Charge entry specialists input:
– CPT codes
– diagnosis codes (ICD-10)
– modifiers
– date of service
– provider information
– number of units
Accuracy at this stage ensures the claim goes out clean. Errors such as missing units, wrong place-of-service codes, or incorrect provider NPI can cause rejections and delayed payments. Charge entry is a crucial component of mid-cycle RCM.
Keywords Added:
✔ charge entry process
✔ CPT codes
✔ ICD-10 coding
✔ medical billing data entry
✔ practice management software
4. Medical Coding: Translating Healthcare Services Into Standardized Codes
Medical coding is the backbone of the medical billing system. Coders translate provider documentation into standardized codes that insurance companies use to process claims. These codes include:
- ICD-10-CM for diagnoses
- CPT for medical procedures
- HCPCS Level II for supplies and equipment
Coders must analyze provider notes, lab results, and procedure reports to choose the most specific and accurate codes. Proper coding ensures appropriate reimbursement, avoids compliance issues, and reduces the risk of claim denials.
Common coding issues include:
– under coding
– up coding
– missing modifiers
– using outdated codes
Successful coders remain updated with annual code changes and payer-specific guidelines to prevent errors and improve claim approval rates.
Keywords Added:
✔ medical coding
✔ CPT and ICD-10 codes
✔ HCPCS codes
✔ up coding and under coding
✔ coding compliance
5. Claim Submission: Sending Clean Claims to Insurance Companies
After coding and charge entry, the claim is prepared for submission. Claims go through claim scrubbing, where software checks for errors such as missing information, inaccurate codes, or formatting issues. Scrubbed claims are then sent electronically through a clearinghouse or directly to the insurance payer.
Insurance companies review the claim for:
– medical necessity
– eligibility
– correct coding
– contracted rates
– possible errors
Clean claims those submitted without errors are processed quickly, leading to faster reimbursement.
Keywords Added:
✔ claim submission process
✔ clearinghouse
✔ electronic claims (EDI)
✔ claim scrubbing
✔ clean claim rate
6. Payment Posting: Recording Insurance and Patient Payments
After the insurance company processes the claim, they send an Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA) showing payment details. Payment posting involves entering these payments into the billing system accurately.
During payment posting, billers:
– apply insurance payments
– record adjustments (contractual obligations)
– bill patients for any remaining balances
– identify payment discrepancies
– flag underpayments or unpaid claims
Payment posting helps maintain accurate accounts and ensures the patient receives a correct bill. It also helps identify trends such as frequent underpayments or payer errors.
Keywords Added:
✔ payment posting
✔ EOB and ERA
✔ insurance reimbursements
✔ medical billing adjustments
✔ patient balance billing
7. Denial Management: Identifying and Resolving Claim Denials
Denial management is one of the most challenging parts of the revenue cycle. Even well-prepared claims can be denied due to clerical mistakes, technical issues, documentation gaps, or payer-specific rules.
Common denial reasons include:
– incorrect patient info
– invalid codes
– lack of prior authorization
– missing documentation
– non-covered services
– eligibility issues
Effective denial management involves analyzing denial codes, correcting errors, submitting appeals, and resubmitting corrected claims. Practices that track denial trends can update workflows to prevent future denials and improve revenue cycle performance.
Keywords Added:
✔ denial management
✔ medical billing denials
✔ claim appeals
✔ root-cause denial analysis
✔ denial prevention strategies
Final Thoughts: Why Understanding the Medical Billing Workflow Matters
The medical billing workflow is a complex but essential process that ensures healthcare providers receive accurate payment for their services. When each step—from patient registration to denial management—is performed correctly, providers experience:
- fewer claim rejections
- faster reimbursement
- improved cash flow
- higher clean claim rates
- better patient satisfaction
Understanding this workflow is crucial for medical billers, coders, and healthcare organizations seeking to strengthen their Revenue Cycle Management performance.
Latest Article
A Complete Guide for Accurate and Faster Reimbursement
Basics of Healthcare Finance: Understanding Revenue and Expenses in US Medical Practices
Smart Billing: How to Optimize Medical Billing for Maximum Efficiency and Revenue

Efficient Billing: How to Streamline Medical Billing for Faster Payments
Medical Billing Terms

Medical Claim Management
Need Help?
Call Us
+6221.2002.2012
(Free Toll)


One Response
It is brilliant knowledge for medical billing basics ,it will be very helpful for freshers in medical billing great work.